Studies from all around the world continue to point to the importance of sleep and how it can vitally affect our overall mental health.
Many of us know the feeling after losing a night of rest, it’s as if zombies were real, and we are the walking dead. When we pull an all nighter, our head likely is pounding, we have poor judgment, our attention has a life span of seconds, our memory is fuzzy, and creative and critical thinking were smart enough to go to bed hours before, leaving us in a sleepless daze. On top of all this, we are likely in a terrible mood.
But after a few cups of coffee and a good night’s rest, all of these symptoms will eventually go away, leaving us feeling healthy and ready to conquer the day, week, month, and years to come. But what if these sleepless nights were actually limiting those years? What if they were affecting our minds not only in the short term but in the long term as well, in a very serious way?
New research has emerged that could potentially link sleep deprivation to Alzheimer’s disease (AD). The studies are ongoing but many key indicators point to a strong correlation between the two.

History of Alzheimer’s

Dr. Alois Alzheimer
In 1906 a woman named Auguste Deter was the first person to be diagnosed with Alzheimer’s disease. For several years, she had been the patient of Doctor Alois Alzheimer. During this time he had observed odd behaviors like memory loss, sleep deprivation, vegetative states, and hallucinations.
With the assistance of two Italian physicians, Dr. Alzheimer examined her brain and found abnormal clumps and tangles in the neural tissue. These are known today as amyloid plaques and tau tangles, two key authenticating factors of a modern Alzheimer’s diagnoses.
“Alzheimer’s is a type of dementia that causes problems with memory, thinking and behavior. Symptoms usually develop slowly and get worse over time, becoming severe enough to interfere with daily tasks.”
Alzheimer’s is a deadly disease that begins with neural damage in the hippocampus, the part of the brain associated with forming memories. As nerve cells continue to lose their connections, plaques and tangles build up, and neurons die, the final stages of Alzheimer’s has set in and the brain has reduced significantly in size.
Poor Sleep Common Among Alzheimer’s Cases
One of the many symptoms of AD is sleep deprivation or a change in sleep patterns. This can include changes in the wake-sleep cycle as well as feeling fatigued during the day. Alzheimer’s patient may also have trouble staying asleep at night or during naps.Progression of Alzheimer’s Disease

“Disturbances in the sleep–wake cycle and circadian rhythms are common symptoms of Alzheimer Disease (AD), and they have generally been considered as late consequences of the neurodegenerative processes. Recent evidence demonstrates that sleep–wake and circadian disruption often occur early in the course of the disease and may even precede the development of cognitive symptoms.”
[2] Experimental and Molecular Medicine
New Science Suggests a Link Between Alzheimer’s and Sleep Deprivation
The Central Nervous system has a waste removal pathway known as the glymphatic system. This functions to remove toxic proteins like beta-amyloid and tau when the body is asleep, particularly during deep non-REM (Rapid Eye Movement) stages of sleep.
Because these toxic proteins have been linked with Alzheimer’s disease, medical professionals have questioned whether or not aggravated sleep patterns could impair the glymphatic system and link sleep disturbances to AD.
Several studies done in the past few years have discovered a connection between sleep loss and the buildup of these plaques in the brain. The result of these studies could potentially associate Alzheimer’s with conditions such as sleep apnea and more generalized sleep deprivation (read more).
The findings of these studies show increased amounts of the toxic protein tau and the metabolic waste product beta-amyloid. A recent Mayo Clinic study of 288 participants 65 and older, found that those who had sleep apnea had 4.5 percent higher amounts of the tau protein in their brain than those participants who had not been observed to have an episode of sleep apnea.A smaller study of 20 participants, ages 22 to 72, done by the National Institutes of Health documented a 5 percent increase in the protein beta-amyloid after participants went about 31 hours without sleep.
The results of these studies and others like them are questioned on both ends, much like “which came first the chicken or the egg” scenario. Is it the increase in brain toxins that causes sleep deprivation? Or are sleep disturbances causing the elevated levels of tau and beta-amyloid proteins?“Disrupted sleep is commonly observed in individuals with symptomatic AD (Peter-Derex et al., 2015) and can be detected in the preclinical stage (Ju et al., 2013; Hahn et al., 2014; Lucey et al., 2019). Moreover, sleep fragmentation, poor sleep quality, and excessive daytime sleepiness have been shown to increase risk of cognitive impairment and eventual dementia in clinical populations (Blackwell et al., 2013; Lim et al., 2013a; Spira et al., 2015, 2018).”
[3] Frontiers in Aging Neuroscience
Escalating Rate of Alzheimer’s
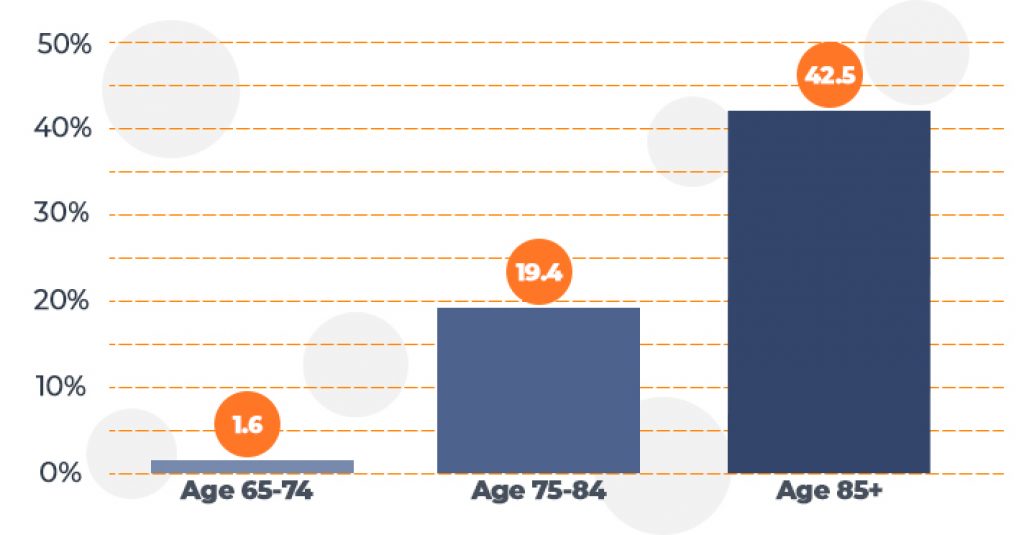
Alzheimer’s disease is not a natural part of aging. Though like many conditions, the risk does go up as people get older. One of the main reasons AD may be escalating so quickly is that people are living longer and the greater the lifespan, the greater the chances are that Alzheimer’s may affect individuals.
“Unless Alzheimer’s can be effectively treated or prevented, the number of people with it will increase significantly if current population trends continue. This is because increasing age is the most important known risk factor for Alzheimer’s disease.”
[4] National Institue of Aging
Experts agree that as people get older, they begin to spend less time in deep, slow-wave non-REM sleep. It is during this restorative phase of sleep that the glymphatic system removes harmful toxins from the brain.
The University of Rochester Medical Center recently performed a sleep study on mice that may help expand current knowledge on the glymphatic pathway.
“The synchronized waves of neural activity during deep slow-wave sleep, specifically firing patterns that move from front of the brain to the back, coincide with what we know about the flow of CSF (Cerebrospinal Fluid) in the glymphatic system,” said Lauren Hablitz, Ph.D., one of the authors of the study. “It appears that the chemicals involved in the firing of neurons, namely ions, drive a process of osmosis which helps pull the fluid through brain tissue.”
This study helps bridge the gap between deep sleep and the lymphatic system. Their research demonstrates how these two correlating factors could potentially influence Alzheimer’s disease as people age.
One question that is developed from this finding is, if people are getting less slow-wave, waste removing sleep as they get older, would these occurrences increase the likelihood of developing Alzheimer’s? Likewise, if there was a way to help increase the time people spend in deep sleep, could this be a preventative treatment to those at risk to AD?
Professionals agree that further research on the topic is needed in order to develop concrete answers, but the evidence suggests there is a correlation between non-REM sleep disturbances and the escalation of AD.
Odds of Developing Alzheimer’s Disease
As more people are being diagnosed with AD, it is only natural that the spending will increase as well. By the year 2050, it is projected that if the disease continues at its current rate, the United States government will be spending more than 1 trillion dollars to prevent and treat Alzheimer’s.
Medicare and Medicaid Spending for People with Alzheimer’s Disease (in billions)
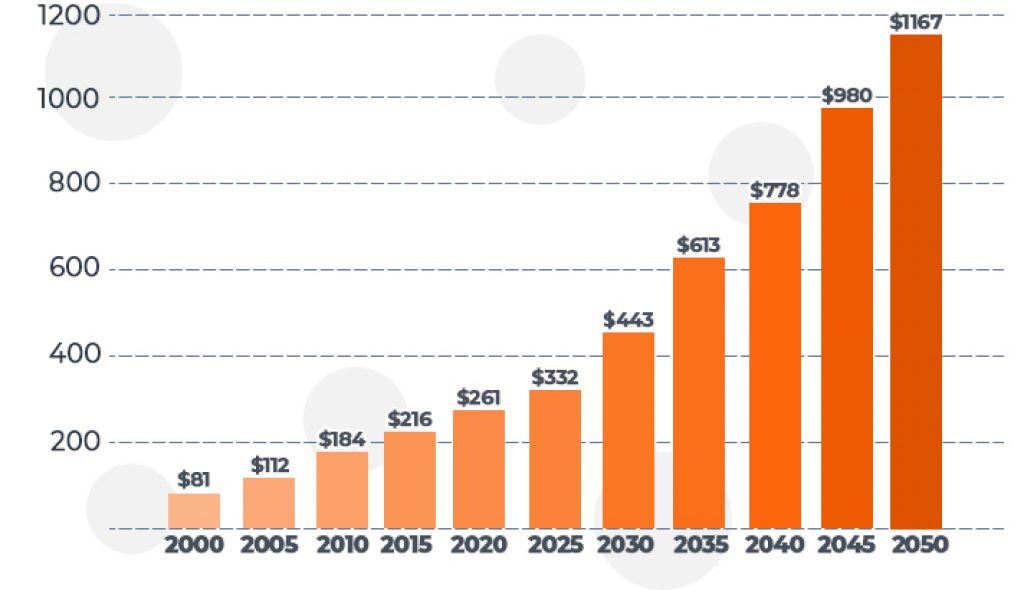
– [5] Alzheimer’s Association
Could Better Sleep Reduce the Rate of Alzheimer’s Cases?
Further research will be needed to know for sure, but evidence suggests that it might. The study performed by the University of Rochester Medical Center indicates that the glymphatic pathway can be exploited by improving sleep patterns, theoretically reducing toxin accumulation in the brain. This would be a hopeful result that could possibly lead to additional clinical tests and trials.
Conclusion
Here is the take away: Alzheimer’s and many other medical conditions could potentially be stopped or slowed down by getting adequate sleep at night. Doing this can drastically improve your health and overall quality of life.
And before you start freaking out (like I did) thinking that you might be at risk for Alzheimer’s because, like most people, you don’t get enough sleep, remember that this research is new and there is still a lot to be discovered.
Here is what you do now: If you are not already, try going to bed tonight, and get between 7 to 9 hours of sleep. Then do it again tomorrow, and the next night, and the next night. And so on…
Not only may this, maybe, possibly fight Alzheimer’s disease, but it should help you feel a good deal better and could help prevent many other medical conditions. Sleep tight!
Sources and References:
[1] What Is Alzheimer’s?, Alzheimer’s Association
[2] Sleep, Circadian Rhythms, and the Pathogenesis of Alzheimer Disease, Experimental and Molecular Medicine
[3] The Interaction Between Sleep and Metabolism in Alzheimer’s Disease: Cause or Consequence of Disease?, Frontiers in Aging Neuroscience
[4] What Is Alzheimer’s Disease?, National Institute on Aging
[5] A National Alzheimer’s Strategic Plan: The Report of The Alzheimer’s Study Group, Alzheimer’s Association

Mark Mattei
Content Writer
About Author
Mark likes to study sleep health, write content, and produce videos on his findings. When he’s not, he’s likely writing the great American screenplay, growing out his beard, or spending time with his family.
Mark is an exclusive side sleeper with broad shoulders who looks for good pressure relief for his hips and shoulders.
Combination Sleeper
