If you serve or have served in the United States military and are currently struggling with sleep, you are definitely not alone. Authors of a military sleep evaluation proposed that “while the prevalence of sleepiness in the military is largely unknown, it is well established that short sleep duration is endemic. The reasons for this include: the demanding nature of their duties, shift work and 24-hour duty periods, deployments and exigencies of military service as well as sleep disorders.”
This study, along with dozens of others, points towards evidence that suggests our military is not sleeping enough.
Whether you’re an active-duty service member, a veteran, or are related to a soldier, this guide is here to help. We’ll explore the prevalence and root cause of sleep issues in the military before covering different treatment options for improving sleep.
Military vs. The General Population:
Who Gets Less Sleep?
Approximately one in three Americans do not get enough rest. Compare this to a number of other studies that report anywhere between 62% and 74% of military personnel are classified as poor sleepers.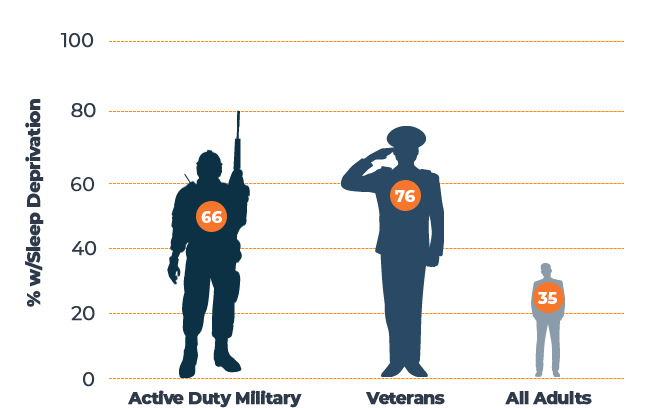
Sources: “Health of the Force” — [2] U.S. Army, “National Veteran Sleep Survey” — [3] My Vet Advisor, “Sleep Facts and Stats” — [4] Centers for Disease Control and Prevention
In one self-assessed report, soldiers averaged around 5.8 hours of sleep in a 24-hour period. This means that 72% of military personnel were getting less than 6 hours of sleep, while another study reported an alarming 42% were getting less than 5 hours of rest per day. To put this into perspective, roughly 65% of American adults say that they get more than 7 hours of sleep each night.
The November 2015 Health and Force report found that only 15% of active-duty soldiers in the army meet the national sleep standards, while an alarming 55% failed to reach any of the defined targets.
Many Veterans are experiencing similar sleep issues as active-duty military – Veterans from all branches averaged just 5.6 hours each night. Another survey found that one in five Veterans gets less than 4.5 hours of rest per night. According to both studies, evidence suggests that between 76% and 89% of Veterans are sleep deprived compared to just 35% of civilians.
Sleep Issues During Deployment and Post-Deployment
How Deployment Affects Sleep
According to one study, pre-deployment troops averaged around 7 to 8 hours of sleep. Post-deployment, the average decreases to 5 to 6 hours.
A study performed by Madigan Army Medical Center found that 58% of nearly 800 military personnel were diagnosed with a sleep disorder. Those who were affected had the following:
Sleep Conditions in Military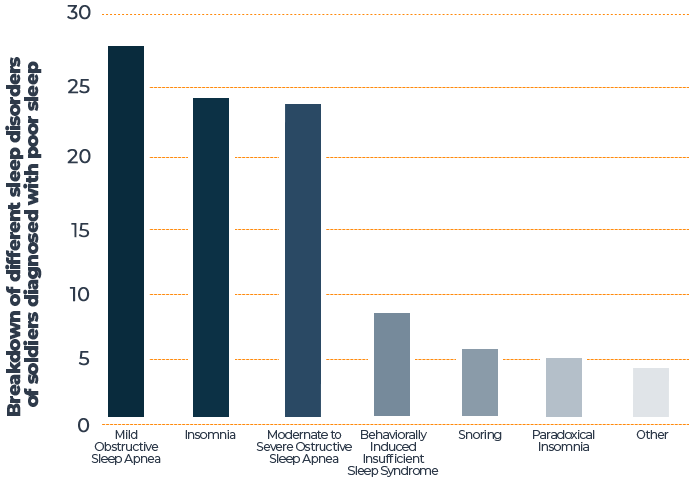
Source: “Sleep Disorders and Associated Medical Comorbidities in Active Duty Military Personnel” — [5] National Center For Biotechnology Information
How Post-Deployment Affects Sleep
Veterans sacrifice their time and talents, often risking their lives to protect and defend their country. Unfortunately, when they step back into their civilian shoes, their problems do not always end. Conditions like depression, anxiety, post-traumatic stress disorder (PTSD), and sleep disorders follow them into their homes.
Sleep deprivation is one of the steepest problems facing our Veterans. Up to 89% of Veterans classify as poor sleepers. A study found that among 9.7 million U.S. Veterans surveyed, the prevalence of sleep disorders had increased six-fold. Another survey found that 54% of respondents enrolled with the Department of Veteran Affairs had been diagnosed with a sleep disorder.
The subjects of both these analyses were just the Veterans who had sought care, which means there are inevitably more Veterans dealing with sleep deprivation that are unaccounted for.
Common Sleep Disorders Among Vets
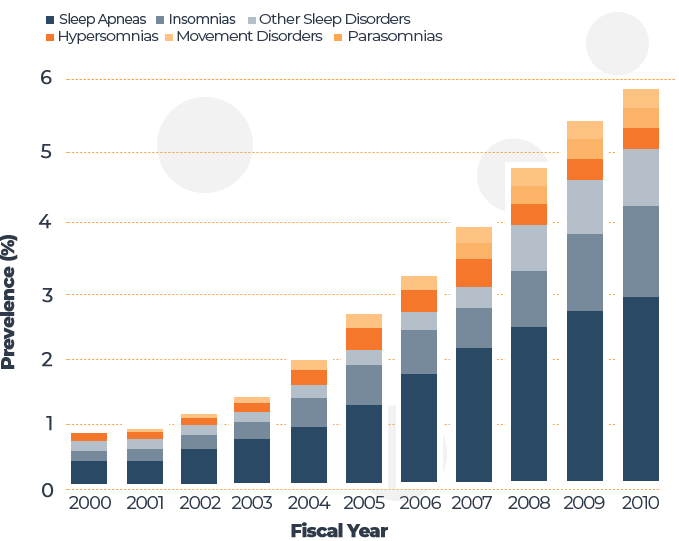
Sources: “The National Veteran Sleep Disorder Study: Descriptive Epidemiology and Secular Trends, 2000–2010” — [10] National Center For Biotechnology Information
Insomnia
“Individuals with insomnia have trouble falling asleep or staying asleep. Insomnia leads to daytime sleepiness, lack of energy, and difficulty focusing.” — National Library of Medicine. [11]
Find Out More: How To Deal With Insomnia
Sleep apnea
“Sleep apnea is a common sleep disorder in which an individual’s breathing repeatedly stops and starts during sleep. Symptoms include unexplained fatigue, mood swings, and snoring.” — Jonathan Jun, M.D.; a pulmonary and sleep medicine specialist at the Johns Hopkins Sleep Disorder Center [12]
Read more about sleep apnea.
Circadian rhythm disorders
Circadian rhythm refers to the natural cycle our bodies go through in a 24-hour period. Also referred to as the “body’s clock”, circadian rhythms are affected by light and darkness, and are crucial for maintaining healthy sleep and wake times.
“Circadian rhythm disorders are disruptions in a person’s circadian rhythm… The key feature of circadian rhythm disorders is a continuous or occasional disruption of sleep patterns. Symptoms include excessive daytime sleepiness, insomnia, and poor work performance.” — Cleveland Clinic [13]
Movement disorders
“Periodic limb movement disorder is a condition characterized by repetitive limb movements during sleep. This can cause daytime fatigue and frequent awakenings during sleep.” — Cleveland Clinic [14]
Hypersomnia
“Hypersomnia is a condition where a person feels excessively tired during the day or sleeps longer at night. It is different from feeling tired due to lack of or interrupted sleep at night…You might fall asleep repeatedly during the day, at inappropriate times such as at work.” — National Institute of Neurological Disorders and Stroke [15]
Nightmares
“Nightmare disorder is when nightmares happen often, cause distress, disrupt sleep, or create fear of going to sleep. You may have nightmare disorder if you have frequent nightmares coupled with daytime fatigue, problems functioning at work, and persistent anxiety or fear.” — Mayo Clinic [16]
Night terrors
“Night terrors, or sleep terrors, are episodes of screaming, intense fear, and flailing while still asleep…Sleep terrors differ from nightmares in that the person remains asleep and rarely remembers anything from the episode .” — Mayo Clinic [17]
Additionally, studies show that “The majority of patients with PTSD, about 50-70%, suffer from recurring distressing nightmares.” — Frontiers in Psychiatry Medical Journal [18]
REM sleep behavior disorder
“REM sleep behavior disorder is when you physically act out your dreams. RBD is a parasomnia, which is a sleep disorder that involves unusual and undesirable physical events or experiences that disrupt your sleep.” — Cleveland Clinic [19]
Sleep paralysis
“Sleep paralysis is a feeling of being unable to move, either at the onset of sleep or upon awakening. During an episode, you’re aware of your surroundings but can’t move or speak. Many people hear or see things that aren’t there (hallucinations), making episodes even more frightening” — Cleveland Clinic [20]
Learn more about sleep paralysis.
Common Conditions Among Veterans That Can Affect Sleep
Traumatic brain injury
11%-23% of deployed troops have suffered mild TBI
“Sleep disturbances after TBI are estimated to occur in 30–70% of head injured patients, often impairing the resumption of normal activities.” — Nathaniel F. Watson, M.D. [21]
Tinnitus
Over 150,000 Veterans were diagnosed with tinnitus in 2015
“Veterans have higher rates of tinnitus than the general public due to the noise levels they encounter while in the service, including gunfire, machinery, aircraft, and much more… Tinnitus is defined as the perception of ringing, hissing, or other sounds in the ears or head when no external sound is present.” [22]
Pain
65.5% of veterans reported having pain in the last three months
“For those who return home with physical wounds, pain management becomes a challenge. Even after injuries are treated, there are still other issues: headaches, neurological pain in ghost limbs, long-term painful conditions like arthritis. Many Veterans dealing with pain may struggle with “painsomnia”, which refers to pain so intense it prevents one from falling asleep.” [23]
Substance Abuse
36%-72% of substance abusers have insomnia
“Traumatic events such as combat exposure and multiple deployments can trigger drug or alcohol use, which all too often lead to addiction.” [24]
PTSD
13.8% of Veterans who served in Iraq and Afghanistan were diagnosed with PTSD
“Post-traumatic stress disorder is a mental health problem that can occur following the experience of a psychologically traumatic event like war, assault, or disaster. The estimated prevalence of PTSD in the general population is 1-9%, among victims with significant trauma the figure is 20–45% and among Veterans, it is 15–20%.” — Sleep Disorders Research Center [25]
Dr. Raj on How PTSD Can Impact Sleep Among Veterans

Depression and anxiety
One study shows that 27%-30% of Veterans have a triple combination of PTSD, anxiety, and depression
“In 2008, the U.S. Department of Veteran Affairs estimated that about one in three Veterans visiting primary care clinics have symptoms of depression.” [26]
Learn more about anxiety and sleep here.
What is the Military Doing to Address Sleep Issues?
Those serving our country are under immense pressure to perform in high-stress situations. Therefore, it comes as no surprise that the majority of soldiers are sleep-deprived.
Service members in general, and those who have deployed, specifically, are at high risk for insufficient sleep duration. This is particularly concerning, given the robust evidence linking short sleep duration with compromised mental and physical health and cognitive impairments, all of which can have a direct impact on operational readiness and servicemember resilience. [6] National Center for Biotechnology Information
What’s the military doing about it? The United States Department of Defense trains personnel to have good sleep hygiene and screens them for possible disorders. While they have taken steps in the right direction, one study by the RAND Corporation suggests that military leaders may be uneducated on the subject and noted several places where sleep health training could be improved.
The same study points out that there are several hurdles to achieving better rest for service members. Those in charge do not necessarily understand how sleep deprivation affects behavior, so there aren’t many policies dedicated to educating soldiers on sleep hygiene. In addition, many of the sleep regulations currently in place are often perceived as mere guidelines. Lack of sleep-health resources, such as instruments used for screening and studying sleep as well as other tools and training, is another problem the military faces.
However, science continues to prove that humans need sufficient sleep to perform at their highest level. We’ve learned that soldiers sleep far less than most other groups of people, yet they’re expected to function at a higher level, often while under immense stress.
This raises the question: Could it be beneficial for the military as a whole to dedicate funding towards sleep education and care? As the U.S. Defense budget is increased, allocating resources towards sleep-health could prove worthwhile.
Sleep Issues During Deployment and Post-Deployment
Studies show how military-induced sleep deprivation makes soldiers and Veterans more prone than the general population to underlying mental illnesses, many of which can lead to conditions like Post Traumatic Stress Disorder (PTSD), substance abuse, and even suicidal thoughts and actions.
The nature of the military leads to less rest. Days as well as nights are often full of assignments and thus, an alarming amount of stress. If physical and mental fatigue were not enough, soldiers are often forced to sleep on a cot, or worse, on the ground, making it feel near impossible to fall asleep.
Here are just a few ways these conditions can affect a soldier.
Decreased Performance and Fatigue
“As sleep debt accumulates, a person’s mood, motivation, attention, alertness, short-term memory, ability to complete routines, task performance (errors of omission more than errors of commission) and physical performance will become more negatively affected.” — Defence Medical Research Institute Ministry of Defence [7]
Heart conditions and cardiovascular disease
“What many people don’t realize is that the amount of sleep you get and when you sleep directly affects your heart health… One of the potentially most dire consequences of these effects is their contribution to heart disease. Poor sleep quality in general, and especially sleep apnea, is associated with an increased risk of high blood pressure.” — Joseph Hill, M.D., Ph.D. [8]
MicroSleep
A microsleep is defined as a brief period of rest that lasts as little as a few seconds and up to 30 seconds at most.
“Soldiers who routinely get less than 7 hours of sleep perform much like a person who is legally drunk. They lose their situational awareness, lose the ability to exercise good judgment and may partake in risky behaviors. They also are at risk of uncontrolled and unintentional sleeping. Microsleep can occur during critical events such as driving, speaking and even walking. Put simply, accidents increase when the total amount of sleep you get each night decreases over time.” — Army Performance Triad [9]
Note: These are only a few conditions that sleep deprivation can cause. Others include headaches, obesity, as well as increased risks for conditions such as diabetes and some cancers.
Moral Reasoning & Decision-Making
A sleep study was performed on officers at both the Norwegian Naval Academy and the Norwegian Army Academy. The experiment tested their moral reasoning under both rested and severely unrested states. The findings of the experiment demonstrated that
The experiment tested their moral reasoning under both rested and severely unrested states. The findings of the experiment demonstrated that “the officers’ ability to conduct mature and principally-oriented moral reasoning was severely impaired during partial sleep deprivation compared to the rested state.”
Insomnia and Suicide
Correlation between Pre-Deployment Insomnia and PTSD
When people think of PTSD, conditions like anxiety and depression might be at the front of your mind. However, new studies show that sleep-related disorders have a closer relationship to PTSD.
In a 2012 study, researchers analyzed a group of U.S. Army soldiers 1 to 2 months before they were deployed to Afghanistan. Overall, 15% reported that they had experienced insomnia within the thirty days pre-deployment. After their return, soldiers who had reported insomnia within this time frame were two times more likely to experience suicidal thoughts and twice as likely to have PTSD than those who had not reported insomnia.
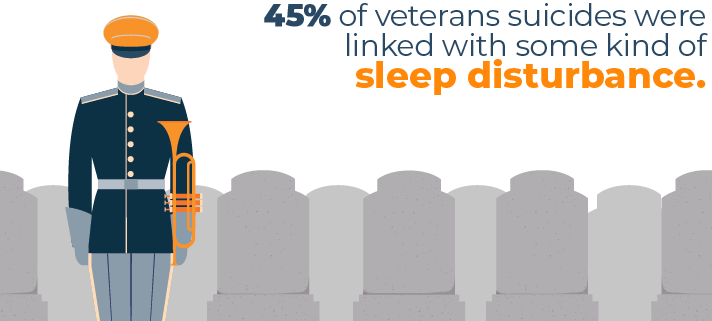
Similar to active-duty soldiers and the relationship between insomnia and suicide, an analysis in 2012 observed that 45% of Veterans suicides were linked with some kind of night-time disturbance.
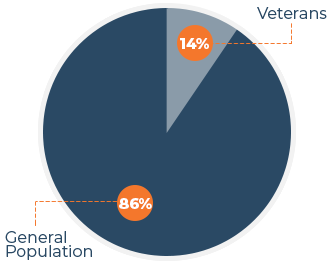
Suicide Rates 2016 –
Veterans vs. General Population
In the U.S., veteran suicides account for 14% of the national suicide rate, but only account for 8% of the total population.
Based off of these numbers, the veteran suicide rate in 2016 was 1.5 times higher than the general population. That means over 6,000 Veterans died by suicide, which is more than soldiers that died over the seven years of Operation Iraqi Freedom (4,423 U.S. military casualties 2003-2010).
If we were to theoretically apply that 45% of veteran suicides from that one study into roughly 6,000 troops, that would total 2,700 suicide deaths related to sleep deprivation.
These studies indicate more than just the prevalence of sleep deprivation among Veterans. The numbers show the devastating effects sleep deprivation has on Veterans as a whole.
A rapidly growing body of literature demonstrates that insomnia is a reliable risk factor of poor clinical outcomes, including PTSD, depression, and/or suicidality, and impedes the recovery process. Thus, efforts for early identification and timely intervention are important goals in order to reduce the impact of deployment on sleep, accelerate recovery from insomnia, and ultimately prevent the onset of psychiatric comorbidities including suicide.
[27] National Center for Biotechnology Information
Treatment Options
Cognitive behavioral therapy
This is the most widely studied form of psychotherapy. It uses two schools of therapeutic approach, cognitive and behavior therapy. Patients work with a mental health counselor who helps them become more aware of the relationship between their thoughts and behaviors.
Relaxation therapy
Teaching the mind to relax can take time, but with time meditation therapies can help Veterans and soldiers clear their heads of troubling thoughts. These can take several weeks or even months to get used to and do not necessarily need to be performed on a daily basis, though this would likely improve results. This technique can be done at any point during the day or week, but taking 20 to 30 minutes to relax right before bed might be most beneficial.
Light therapy
For people who have Circadian Rhythm Disorders, light therapy can help re-establish the body’s internal clock through specialized lights. This could be beneficial for Veterans who have severe jet lag, soldiers who work irregular shifts, night shifts, or soldiers and Veterans who otherwise sleep when they should be awake and vice versa.
Therapy Dogs
Therapy dogs are great for all sorts of tasks. They can be especially good for Veterans with PTSD. These animals can help reduce the trauma associated with triggering events. After completing extensive training, therapy dogs can recognize signs of pain, fear, and anxiety in Veterans and provide comfort.
CPAP Therapy
CPAP machines are used to treat people who have sleep apnea. This method increases air pressure in the trachea to prevent the airway from collapsing as the sleeper inhales. This form of therapy may also help reduce nightmares and other key symptoms associated with PTSD.
Circadian rhythm adjustments
This can be done in correlation with light therapy by retraining the mind on when it should be asleep and when it should be awake. This technique helps to re-establish the body’s internal clock in order to more successfully induce proper rest.
Addiction rehabilitation
Addiction rehab often uses psychotherapeutic methods to help users quit or reduce substance use and abuse. Substance abuse is often influenced by or causes other issues like depression, anxiety, and PTSD. Addiction Rehab is designed to show Veterans that they are in control of their lives so they can better control their addiction.
Why Do Many Soldiers and Vets Not Seek Treatment?
The support of family, friends, and medical professionals is important, especially to a soldier or veteran with PTSD or a related condition. Sadly, the hard truth is that so many of these men and women do not feel that they have this support.
Researchers Adam D. Bramoweth, Ph.D. and Anne Germain, Ph.D. agree that soldiers need encouragement. They wrote in their report, “In addition, family and social support are critical elements of successful reintegration and/or recovery. Thus, research and clinical efforts directed at military family members may be important components in providing the care needed and promoting health and recovery among service members and their families.”
Here is another major problem: Veterans often recognize something is wrong but they do not always understand what is happening to their minds or bodies, so may not take action. A University of Minnesota study observed over 7,600 Veterans and found that when attentive care is delayed, individuals often fail to seek help in time.
Dr. Michele Spoont, a clinical and research psychologist at the Minneapolis VA Health Care System, said that “Part of what we’re doing at VA with initial screening is to address this. If we can get a Veteran into a specialist that same day, it enhances their chance of success.”
She also indicated that having the belief that they can actually get help is a huge determining factor. “Veterans have to believe they can get better, that the treatment works,” Spoont said. “and they need to believe that they can do it.”
Veterans and soldiers are accountable for their own health, but it is becoming increasingly apparent that family, friends, and medical providers play a pivotal role in helping service members find the help they need to achieve better rest and mental health. These conditions are not merely physical but often have psychological and social effects. Therefore, it’s crucial that these support systems not only encourage service members to get treatment, but help them at every step along the way.
“Given the multiple health concerns these soldiers face, and the rise in suicides in returning Veterans, it is critical that we look for viable strategies to improve their overall health.” — Jacob Collen, M.D., Critical Care and Sleep Medicine, Walter Reed National Military Medical Center [28]
Tips for Better Sleep & Resources for Veterans
First, it helps to realize that you are not alone. Take comfort in the fact that there are many resources and treatments available to you as well as trained medical professionals who specialize in working with soldiers and vets with these issues.
“For many people, simply improving their sleep habits will help. Try to avoid caffeine, nicotine, and exercise in the hours leading up to sleep; avoid using alcohol as a sleep aid; don’t go to bed hungry; try to keep your bedroom dark and quiet; use sleep masks and/or earplugs if needed; and keep your smartphone/devices out of bed.” — Captain Jeffrey Osgood
Establishing a good bedtime routine could be a great place to start. According to Harvard Medical School, a well-practiced routine is key. Develop a nightly routine that helps prepare both the body and mind to fall asleep.
Other tips include:
- Take a warm bath close to bedtime
- Listen to relaxing music or an audiobook before bed
- Do some light reading
- Turn down or dim the lights in the hours before bedtime
- Keep your phone outside of your bedroom while you rest
- Refrain from using screens in the hour before bedtime
Bedtime isn’t the only tip you can implement healthy sleep habits. Proper sleep hygiene really starts in the daytime.
Daytime tips include:
- Avoid caffeinated drinks close to bedtime or late in the afternoon
- Refrain from taking naps longer than 30 minutes
- Try to exercise often
- Expose yourself to sunlight soon after waking up
- Make a “worry list” where you write down everything that’s on your mind so these thoughts are less likely to keep you awake at night
If these solutions do not help improve your rest, please do not hesitate to reach out and seek medical attention from credible sources. You don’t have to be alone with this struggle, and there are many people trained to help you.
If these solutions do not help improve your rest, please do not hesitate to reach out and seek medical attention from credible sources. You don’t have to be alone with this struggle, and there are many people trained to help you.
Resources
If you’re a Veteran in crisis or want to help a Veteran, below are two ways to contact the Veterans Crisis Hotline.
The White House VA Hotline is not a crisis line. This helps to provide extensive training on VA programs and services. This line works with the aforementioned Veterans Crisis Hotline for at-risk Veterans.
The National Veterans Foundation is staffed by Veterans for Veterans. This service provides crisis management and general direction for Veterans and their families.
The VA offers an online course on insomnia:

Mark Mattei
Content Writer
About Author
Mark likes to study sleep health, write content, and produce videos on his findings. When he’s not, he’s likely writing the great American screenplay, growing out his beard, or spending time with his family.
Mark is an exclusive side sleeper with broad shoulders who looks for good pressure relief for his hips and shoulders.
Side Sleeper
References:
[1] “Follow Me”; p. 279. Major General Aubrey Newman. 1981
[2] “Health of the Force”. U.S. Army. Last modified November 2015.
[3] “National Veteran Sleep Survey”. PudMed. Last modified July 1, 2016.
[4] “Sleep Facts and Stats”. Centers for Disease Control and Prevention. Last modified May 15, 2024.
[5] “Sleep Disorders and Associated Medical Comorbidities in Active Duty Military Personnel”. National Center for Biotechnology Information. Last modified Feb 1, 2013.
[6] “Sleep in the Military – Promoting Healthy Sleep Among U.S. Service Members”. National Center for Biotechnology Information. Last modified November 30, 2015.
[7] “Effects of Sleep Deprivation with Reference to Military Operations”. National Center for Biotechnology Information. Last modified January 26, 1997.
[8] “To Sleep, Perchance to Lower Your Heart Disease Risk”. U.S. Southwestern Medical Center. Last modified July 5, 2016.
[9] “What to Know About Sleep Deficiency”. Army Public Health Center. Last modified September 27, 2022.
[10] “The National Veteran Sleep Disorder Study: Descriptive Epidemiology and Secular Trends, 2000-2010”. National Center for Biotechnology Information. Last modified July 1, 2016.
[11] “Insomnia”. National Library of Medicine. Last modified December 4, 2018.
[12] “The Dangers of Uncontrolled Sleep Apnea”. John Hopkins University. Last modified 2024.
[13] “Circadian Rhythm Disorders”. Cleveland Clinic. Last modified April 1, 2020.
[14] “Periodic Limb Movement Disorder in Adults”. Cleveland Clinic. Last modified July 21, 2012.
[15] “Hypersomnia”. National Institute of Neurological Disorders and Stroke. Last modified January 20, 2024.
[16] “Nightmare Disorder”. Mayo Clinic. Last modified June 5 , 2021.
[17] “Sleep terrors”. Mayo Clinic. Last modified April 23, 2021.
[18] “Disturbed Sleep in PTSD: Thinking Beyond Nightmare”. Frontiers in Psychology. Last modified November 24, 2021.
[19] “REM Sleep Behavior Disorder (RBD)”. Cleveland Clinic. Last modified November 22, 2022.
[20] “Sleep Paralysis”. Cleveland Clinic. Last modified October 18, 2021.
[21] “Traumatic Brain Injury and Sleep Disorders”. National Center for Biotechnology Information. Last modified November 1, 2013.
[22] “Tinnitus is Number One Disability for Veterans”. Military.com Network. Last modified July 15, 2022.
[23] “Why Our Veterans Can’t Sleep”. SleepApnea. Last modified July 11, 2022.
[24] “Why Veterans Turn to Drugs and Alcohol”. Addiction Center. Last modified May 4, 2015.
[25] “Sleep disturbances in veterans with chronic war-induced PTSD”. National Center for Biotechnology Information. Last modified July 2016.
[26] “Depression”. U.S. Department of Veterans Affairs Office of Research and Development. Last modified January 15, 2021.
[27] “Deployment-Related Insomnia in Military Personnel and Veterans”. National Center for Biotechnology Information. Last modified October 1, 2014.
[28] “Vets with PTSD and sleep apnea less likely to use CPAP”. Sleep Education. Last modified December 10, 2012.
